How Do You Know if Your Acdf Implant Didnt Take
Abstract
Purpose
Inductive cervical discectomy and fusion (ACDF) has proven constructive in treating radicular arm pain. Mail service-operatively, cervical spine stability is temporarily challenged, just information on bony fusion and speed of fusion are ambiguous; optimum evaluation method and criteria are debated.
Aim
To report bony fusion accomplishment and to obtain an overview of methods to evaluate fusion.
Methods
A literature search was performed in PubMed and Embase. Included studies had to written report original data apropos one- or 2-level ACDF with intervertebral device or bone graft, where bony fusion was assessed using CT scans or Ten-rays.
Results
A total of 146 articles comprising 10,208 patients were included. Bony fusion was more often than not defined as "the presence of trabecular bridging" and/or "the absence of move". Fusion was achieved in 90.ane% of patients at the last follow-up. No gilded standard for assessment could be derived from the results. Addition of plates and/or cages with screws resulted in slightly higher accomplishment of fusion, but differences were not clinically relevant. Eighteen studies correlated clinical outcome with bony fusion, and 3 found a significant correlation betwixt achievement and better clinical event.
Conclusions
In approximately xc% of patients, bony fusion is accomplished ane year after ACDF. As there is no generally accepted definition of bony fusion, different measuring techniques cannot exist compared to a aureate standard and it is impossible to determine the nearly accurate method. Variations in study pattern hamper conclusions on optimising the charge per unit of bony fusion by pick of material and/or additives. Insufficient attention is paid to correlation betwixt bony fusion and clinical outcome.
Graphical abstract
These slides can be retrieved from electronic supplementary material.
Introduction
Anterior cervical discectomy and fusion (ACDF) is a commonly used procedure to decompress cervical spinal fretfulness or the cervical medulla. The "discectomy" refers to the removal of the intervertebral disc including the herniated part to provide decompression of the nervous tissue. The "fusion" part refers to the additional surgical procedure to stabilize the two adjacent vertebrae which will, theoretically, be compromised afterwards removing the intervertebral disc. In order to provide surgical fusion, information technology is usual care to place an intervertebral device, like a bone graft or a cage, between the vertebra to supplant the disc tissue and to maintain foraminal peak. This procedure can be accompanied by anterior plating, which is assumed to add to the stability of the spine. Subsequent "bony fusion" is deemed to follow upon consolidation of the bone between the adjacent vertebrae through and along the intervertebral device. The intervention is regarded to lead to solid arthrodesis and to carry minimal surgical risks [i,2,3]. It is slightly confusing that "surgical fusion" and "bony fusion" are in general both referred to every bit "fusion".
Autologous iliac os grafts too every bit cages made from titanium, polyether ether ketone (PEEK) and diverse other materials are normally used as intervertebral devices. Although cages tin differ in shape and material, they are all intended to maintain height and to add to immobilization of the degenerated move segment [4].
Business firm immobilization is merely effectuated once bony fusion has been accomplished. Anterior discectomy temporarily challenges the stability of the cervical spine mail-operatively, and this tin can theoretically atomic number 82 to kyphotic malalignment [5], which tin can give rise to cervix disability and pain and, ultimately, to neurological deficits. In order to avert these complications, patients' daily activities are restricted until bony fusion has been achieved.
However, knowledge nearly the process of bony fusion is express. Firstly, it is debated what the timing of bony fusion is subsequently a discectomy was carried out. Secondly, the method to judge bony fusion is non equivocal. Finally, the correlation betwixt bony fusion and clinical outcome is unknown.
The primary objective of this systematic review is to study the process of bony fusion and to obtain an overview of methods to evaluate bony fusion. Secondary objectives are to compare results based on evaluation methodology, cage or graft textile and addition of bone stimulating agents, and to assess whether there is a correlation between clinical effect and bony fusion accomplishment.
Methods
Data searches and study selection
To obtain all relevant literature, the electronic databases PubMed and Embase were searched on 14 Jan 2016. The search strings presented in Tabular array 1 were used. Co-ordinate to PRISMA guidelines, ii of the authors (IN and MTK) individually and independently screened the articles for predefined inclusion criteria. These were stated equally follows:
-
The article was published in English or Dutch;
-
The article was an original report presenting primary data;
-
The commodity was published on or after 1 Jan 2000;
-
The study had a minimum of 10 patients;
-
The study focused on the cervical spine (C2-Th1);
-
The study presented patients undergoing a 1- or 2-level inductive cervical discectomy and fusion with an intervertebral device (exempting prostheses) or a bone graft;
-
The included patients did non undergo revision surgery or surgery equally treatment for trauma;
-
The method of assessing fusion was described;
-
The report assessed fusion with CT scan or X-ray;
-
The commodity was published in a peer-reviewed journal.
Only studies that the evaluators reached a consensus on were included. If needed, a third reviewer (CVL) was consulted.
Quality assessment
To assess the quality of the selected studies, the studies were evaluated with the aid of an adjusted version of the Dutch Cochrane Center checklist for cohort studies, presented in Table ii. The methodological requirements and objectives of these studies were closely evaluated. This was done individually and independently by 2 reviewers (IN and CVL). Studies were assessed on selection bias, outcome bias and follow-upward bias, each category accounting for a maximum of 3 points. In total, a study could be awarded a maximum of nine points. Studies were so divided into a low (five–9 points) or high (four or less points) risk of bias group using a method adjusted from Furlan et al. [vi].
Data extraction
All data from the included studies were analysed, and data regarding the following items were extracted:
-
Number of participating patients;
-
Mean fourth dimension and range of follow-up;
-
Pct of fusion at three, 6, 12 and 24 months and at last follow-up;
-
Method of measuring bony fusion;
-
Use of os growth stimulation;
-
Distribution of patients over different implant types;
-
Apply of plate and/or screws;
-
Clinical outcome and correlation to bony fusion;
-
Contact area and height of the implant.
Statistical analysis
Descriptive analyses were performed using paired t-tests, and dichotomous data were analysed using Chi-foursquare tests with Yates' correction. P values of less than or equal to 0.05 were considered statistically meaning.
Clinical relevance was assessed using the method described past Ostelo et al. [7], who defined absolute cut-off values for multiple clinical outcome measures and proposed a minimal clinically important divergence (MCID) as an improvement of thirty% or more than in respect of the baseline value as a general rule.
Results
Characteristics of included studies
Through our search, 1421 unique studies were identified. Later on matching these to our inclusion criteria, 146 studies were included. The most common grounds to exclude studies were as follows: patients did not undergo ACDF, bony fusion was not properly described, and patient numbers were also modest, as shown in Fig. 1.
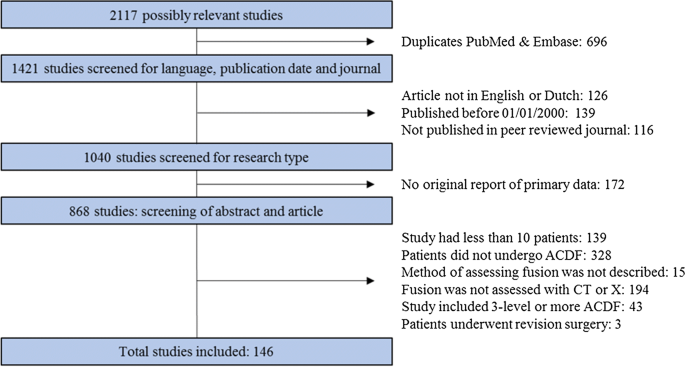
Flow chart of excluding studies. ACDF anterior cervical discectomy and fusion
Combining all studies resulted in a accomplice of 10,208 patients, of whom 3200 received a os graft (including allogenic and autologous bone), 4671 received a polyether ether ketone (PEEK) cage, 348 received a poly(methyl methacrylate) (PMMA) cage, 239 received a carbon fibre muzzle, and 1750 received a titanium muzzle (Fig. 2).
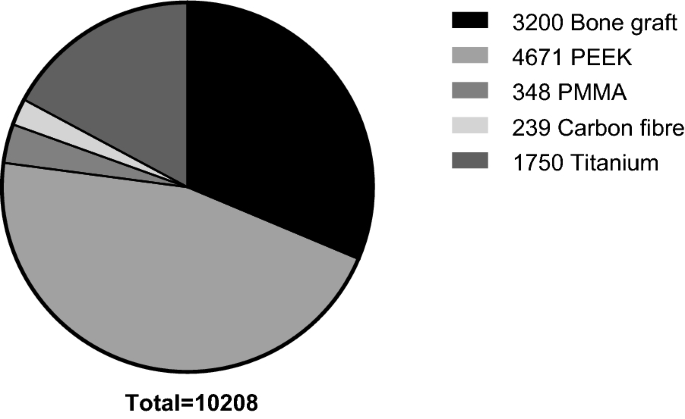
Distribution of implants over patients. PEEK polyether ether ketone. PMMA poly(methyl methacrylate)
Take a chance of bias
A total of 119 studies were assessed to take a low risk of bias, and 27 studies showed a loftier take a chance of bias. When comparing studies with a depression and high risk of bias, the difference mainly seems to exist due to outcome and follow-upwardly bias, since studies with a loftier take chances of bias by and large did not separate follow-up into multiple moments in fourth dimension and did not investigate the correlation between clinical outcome and bony fusion.
Bony fusion
Among many other definitions, bony fusion was most usually divers every bit the presence of trabecular bridging on X-rays or CT scans and/or absence of motion on flexion/extension radiographs. Realization of bony fusion was mostly reported at the final follow-up moment (FFU). The median fourth dimension to FFU was 20.5 months, with a range of iii–408 months. At FFU, studies report accomplished bony fusion in a mean of 90.one% of patients, ranging from i study reporting 30% [viii] to studies reporting 100% [9,ten,11,12,xiii,14,fifteen,16,17,xviii,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,xl,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67]. Studies with a high risk of bias reported statistically significantly higher numbers of patients in which bony fusion was accomplished than studies with a low risk of bias (94.0% and 89.4%, respectively; p < 0.0001). The rate of bony fusion (accomplishment of fusion in a particular patient over time) was studied in approximately one-half of the included manufactures, in which accomplishment of bony fusion was measured at three, vi, 12 and 24 months follow-up (Table iii, Fig. 3) [4, 8,9,10,11, thirteen, 15,16,17, 20, 21, 23,24,25, 27, 30,31,32, 34, 38, 40,41,42, 45, 47,48,49,fifty,51, 54, 55, 57, 59,60,61,62,63,64,65, 67,68,69,lxx,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,xc,91,92,93,94,95,96,97]. Significantly college bony fusion accomplishment rates are observed subsequently longer periods of follow-upwards; however, the difference in accomplishment of bony fusion betwixt 12 months and 24 months follow-up is non clinically relevant.
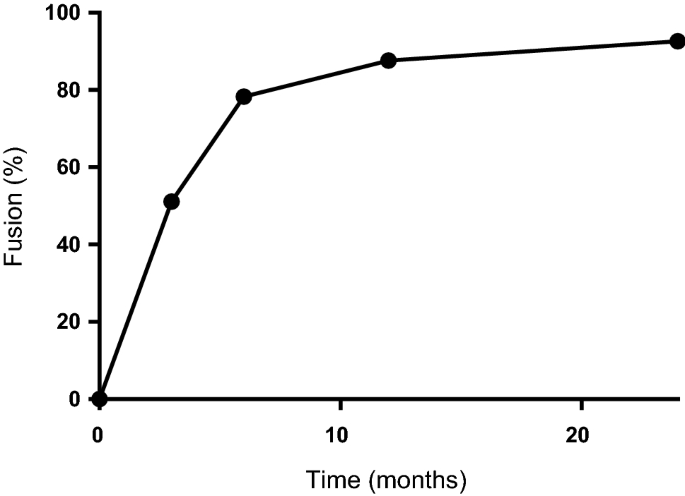
Fusion rate over time
Methods of measuring bony fusion
Trabecular bridging as a sign of achievement of bony fusion was determined in 26 studies evaluating CT scans and in 63 studies evaluating apparently antero-posterior and/or lateral 10-rays. Motion on lateral flexion/extension X-rays as a sign of achievement of bony fusion was determined in 55 studies. In 17 studies, the angulation changes at the target level were measured, and in 11 studies, the difference in interspinous distances upon flexion and deflexion was measured. In 27 studies, the method was not further divers. At FFU, bony fusion was accomplished in 90.1% of patients in studies using CT scanning, bony fusion in studies using plain X-rays was 88.3%, and bony fusion in studies using flexion/extension Ten-rays was 91.vii% (Table 4). The cut-off points in angulation changes and differences in interspinous distances on flexion/extension 10-rays vary between articles (Table 5). This did, still, not lead to dissimilar bony fusion percentages for the angulation studies, only did lead to differences in the interspinous distance studies. Remarkably, fusion percentages were college in those studies that allowed 0-mm difference as an upper border for move in contrast to those that allowed upward to 3-mm movement.
Measuring bony fusion past judging trabecular bridging on plain Ten-rays resulted in significantly lower bony fusion achievement than using flexion/extension Ten-rays (p < 0.0001). In that location was no statistically significant difference in bony fusion achievement comparison trabeculae on CT scans and flexion/extension X-rays (p = 0.06) or trabecular judgment on CT scans and plain X-rays (p = 0.077). A subgroup analysis was performed with the studies measuring fusion at three-, 6-, 12- and 24-month follow-ups (Fig. 4). Gradual increase in the patients that attained bony fusion over the range of the yr afterward surgery is observed. Again, significantly higher bony fusion accomplishment rates are observed afterward longer periods of follow-upward, though the difference in accomplishment of fusion betwixt 12-calendar month and 24-calendar month follow-ups is again not clinically relevant.
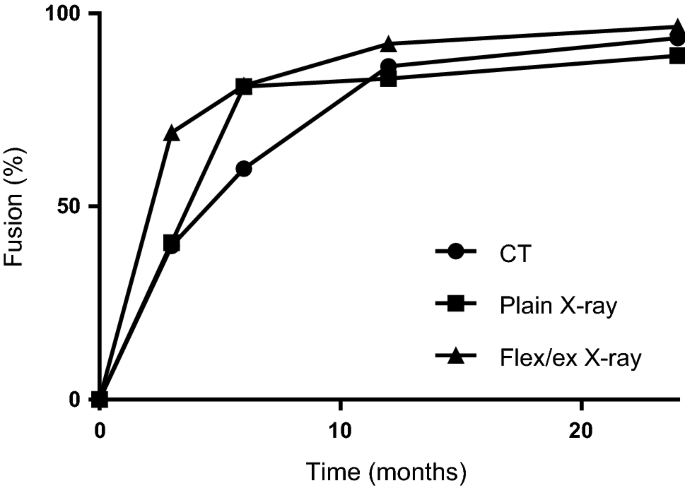
Fusion rate over fourth dimension, stratified per radiologic technique
In 38 of the 146 articles, it was mentioned whether the radiographs were analysed by a radiologist or a clinician. In 26 of these, assay was performed by a radiologist [10, 13, 20, 24, 32, 49, 50, 54, 57, 58, 64, 74, 85, 94, 97,98,99,100,101,102,103,104,105,106,107,108]. They institute fusion was accomplished in 93.5% of patients later on a median follow-up of 23 months. In the other 12 articles, the analysis was performed by a clinician, usually a neuro- or orthopaedic surgeon [12, 29, 35, 61, 67, 69, 87, 92, 96, 109,110,111]. They found fusion was accomplished in 85.5% of patients afterward a median follow-up of 23 months. This deviation in fusion accomplishment was statistically significant (p < 0.0001).
Inter-observer variability was only scarcely documented and could therefore not be analysed.
Correlation fusion and type of implant
At FFU, bony fusion was achieved in 91.iv% of patients with os grafts, in 89.1% of patients with PEEK-cages, in 83.four% of patients with PMMA-cages, in 92.9% of patients with carbon fibre cages and in 91.3% of patients with titanium cages (Table half-dozen). As the median fourth dimension to FFU varied greatly, the different bony fusion percentages cannot be compared.
Correlation bony fusion and use of plates and/or screws
There were 3971 patients who received a plate in add-on to the implant. At FFU, bony fusion was reported in 91.iv% of patients. In that location were 499 patients who received a cage with screws fastened (no plate). At FFU, bony fusion was achieved in 96.6% of these patients. A total of 5738 received a stand-alone implant, without addition of a plate and/or screws. At FFU, the bony fusion rate in these patients was 88.6% (Table 7). In patients treated with a cage with screws attached (no plate), the bony fusion achievement was significantly higher than in patients treated with stand-alone implants and implants with plates (p < 0.0001). In patients treated with stand-alone implants, bony fusion accomplishment was also significantly lower than in patients treated with implants with plates (p < 0.0001). These differences can, yet, not exist concluded to be clinically relevant.
Using bone growth stimulation
The different types of os growth stimulating agents that were used are autologous os in 3985 patients, allogenic bone in 690 patients, freeze-dried cadaveric allogenic bone in 1188 patients, β-tricalcium phosphate in 474 patients, plasmapore coating in 424 patients, hydroxy-apatite in 311 patients, no filling in 1724 patients and 17 other types of bone growth stimulating agents spread over 1412 patients (Fig. v). The distribution of accomplishment of bony fusion over the dissimilar types of agents is shown in Table 8. As the median time to FFU varied greatly, the unlike bony fusion results cannot be compared.
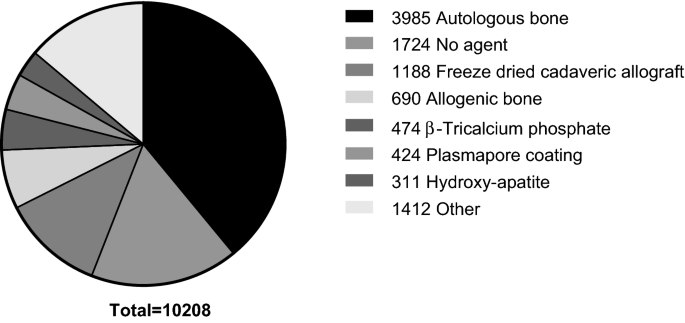
Distribution of bone growth stimulating agents over patients
Correlation of bony fusion and elevation and surface of implant
Dimensional aspects of the implants were described in 19 studies [19, 27, 42, 45, fifty, 51, 53, 72, 74, 77, 81, 85, 94, 111,112,113,114,115,116]. Only the written report by Yoo et al. [116] assessed these aspects in relation to accomplishment of bony fusion. This report had a depression risk of bias and establish no correlation between a cage height of more 7 mm and the absence of bony fusion (odds ratio 3.852; p = 0.101).
Correlation between bony fusion and clinical outcome
Clinical outcome was assessed in relation to bony fusion in 18 studies (Tabular array 9) [25, 37, 40, 63, 84, 95, 105, 107, 109, 112, 116,117,118,119,120,121,122,123]. Of these, 17 studies had a low risk of bias and i written report had a high risk of bias. Out of these 18 studies, 3 found a statistically significant correlation between the occurrence of bony fusion and a good clinical outcome [109, 120, 122]. The other 15 studies did not find a correlation betwixt bony fusion and clinical outcome. Accomplishment of bony fusion in studies that did find a correlation was significantly lower than in studies that did not find a correlation (69.three% versus 89.8%, p < 0.0001). None of these studies correlated clinical outcome with achievement of bony fusion at different time points.
The study by Klingler et al. [109] retrospectively compared patients treated with PEEK and PMMA implants. Clinical outcome was evaluated using the visual counterpart calibration (VAS), the cervix disability index (NDI), the short-form 36 health survey (SF-36) and the patient satisfaction index (PSI). In patients with a PMMA implant, the fusion accomplishment later on a median FFU of 46 months was 47.ane%. Fused patients showed a statistically significant better physical component summary of the SF-36 than not-fused patients (p = 0.024). As the MCID for this measure is 15 [vii], and the accented difference between fused and non-fused patients is 9.2, this difference was not deemed clinically relevant. There was no correlation between bony fusion and other clinical issue measures. In patients with a PEEK implant, fusion was accomplished in 62.2% of patients after a median FFU of xvi months. There was no correlation with any of the clinical outcome measures.
The study by Schroder et al. [120] prospectively studied patients treated with titanium cages and evaluated clinical consequence using Odom's criteria. At FFU (median twenty months), fusion was accomplished in 74.0% of patients. The occurrence of fusion was correlated with splendid and good results, whereas the absence of fusion was correlated with satisfactory and poor results (p = 0.0364). When using Odom's criteria, an MCID cannot be established; therefore, clinical relevance could not exist assessed.
The report by Wright et al. [122] prospectively studied patients treated with autologous bone grafts and evaluated clinical issue using VAS scores for neck pain and arm pain. At FFU (median 12 months), fusion was accomplished in 82.ix% of patients. The absence of fusion was correlated with higher VAS scores for neck hurting. Such correlation was not institute for VAS arm pain. Accented values were not provided in this article; therefore, clinical relevance could non exist assessed.
Give-and-take
Afterward ACDF surgery, bony fusion is achieved in approximately 90% of patients subsequently a median follow-upwards fourth dimension of 20.5 months. Bony fusion rate studies demonstrate approximately 50% of fusion after 3 months, 75% later on 6 months and ninety% from 12 months on. The differences between 12 and 24 months of follow-up are not clinically relevant in the overall group, or when stratified per radiologic technique. From this, it can be concluded that 12 months of follow-up is sufficient.
Methods to determine achievement of bony fusion seem to influence the judgement of bony fusion. Plain X-rays consistently testify lower bony fusion results, even after a longer period of follow-up, and fusion results are too influenced by choosing cutting-off levels for assessment of bony fusion. Comparable fusion results were institute in comparing trabeculae on CT scans and move on flexion/extension X-rays. As in that location is no generally accustomed definition of bony fusion, the different techniques cannot be compared to a gilded standard and information technology is not possible to decide which method is more accurate.
A pregnant correlation was found betwixt fusion accomplishment and whether the imaging was analysed by a radiologist or a clinician. Since the manufactures used in this analysis did non provide additional information on this topic, and none of the articles compared radiologists and clinicians, no explanation towards this difference can be given.
The lack of a mostly accepted definition of fusion is due to the absence of studies that compare fusion in an intervention group with fusion in command groups. Observing bridging of bone trabeculae on X-ray or CT scans is a qualitative measure. Measuring movement on flexion/extension is quantitative and can serve equally a method to develop a gold standard. Ouchida and colleagues [124] claim that flexion–deflexion is more accurately measured on dynamic CT scans in comparison with dynamic 10-rays, though once again a control grouping is lacking. A solution could be to consider "the definite fusion group" in a group of patients treated with an intervertebral device. The "definite fusion group" may be formed by patients that demonstrated overgrowth of bone along and through the device. If those patients serve every bit controls for the other patients, the variation around the 0 degree or 0-mm motility measure, owing to the measuring method, could be established. This can help in establishing a critical value above which the absence of fusion could exist defined.
Another method was introduced by Johnsson and colleagues [125], who introduced metallic markers in the adjacent bony structures to enable observing movement of the vertebrae. Nevertheless, the accuracy was express to 0.five–0.7 mm and 0.v–ii degrees in this study, which was performed in the lumbar spine. Therefore, it seems inadequate to use a cut-off value of 2 degrees to determine on fusion in the cervical spine, similar some of the articles included in this review accept done.
A minority of studies (northward = 18) examined the correlation between achievement of bony fusion and clinical outcome. Only 3 studies demonstrated a correlation between the absenteeism of fusion and worse clinical result, 15 studies did not observe a statistically significant correlation. Studies that did find a correlation had lower bony fusion rates than studies that did non observe a correlation, which could mean that the studies that did not find a correlation did not have enough ability to statistically appraise a correlation betwixt fusion and clinical upshot. Furthermore, none of these studies correlated clinical issue with accomplishment of fusion at different time points. It would be interesting to examine improvement of clinical effect correlated with accomplishment of bony fusion over time. A recent report did demonstrate a correlation between the absenteeism of fusion and neck pain and considered ii time-points [124]. Patients with fusion at 6 months had less cervix pain than without fusion at half dozen months, and patients with fusion at 12 months had less neck pain than those without fusion at 12 months. However, the number of patients studied was relatively low. Besides, the deviation in cervix pain betwixt months 6 and 12, nor the difference in fusion, nor the correlation between those 2 was studied.
In future studies, it is recommended to evaluate clinical condition in correlation with bony fusion in an before phase of the fusion process, when fusion is not yet accomplished in the majority of patients. Conclusions on the correlation of bony fusion and clinical status cannot exist drawn based on the bachelor literature.
Articles with loftier hazard of bias reported higher percentages of bony fusion achievement than articles with low hazard of bias. In articles with a high chance of bias, the method of measuring bony fusion was frequently not described, therefore, the higher fusion rates tin can be due to improper determining of bony fusion.
When comparing different types of implants, os growth stimulating agents, plates or cages with screws and dimensional aspects of the implant, minor statistically pregnant differences are found in bony fusion accomplishment, which do not reach clinically relevant numbers, in regard to the MCID. Small differences in bony fusion results volition likely non be of importance, if a correlation with clinical outcome cannot be established.
Conclusion
Fusion as a long-term result after ACDF is satisfactory, merely lack of a mostly accustomed definition of bony fusion and differences in study blueprint hamper conclusions on optimising the rate of bony fusion by selection of textile and/or additives. Overall, information technology can be concluded that 12 months of follow-up afterward ACDF is sufficient.
References
-
Cloward RB (1958) The inductive approach for removal of ruptured cervical disks. J Neurosurg 15(6):602–617. https://doi.org/x.3171/jns.1958.xv.6.0602
-
Fowler SB, Anthony-Phillips P, Mehta D, Liebman G (2005) Health-related quality of life in patients undergoing inductive cervical discectomy fusion. J Neurosci Nurs J Am Assoc Neurosci Nurses 37(2):97–100
-
Smith GW, Robinson RA (1958) The treatment of sure cervical-spine disorders past inductive removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40-A(3):607–624
-
Lee CH, Hyun SJ, Kim MJ, Yeom JS, Kim WH, Kim KJ, Jahng TA, Kim HJ, Yoon SH (2013) Comparative analysis of 3 dissimilar construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, and muzzle plus plating. J Spinal Disord Techn 26(2):112–118. https://doi.org/x.1097/BSD.0b013e318274148e
-
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt G, Scholz Chiliad, Harders A (2006) Subsidence of the wing titanium cage afterward anterior cervical interbody fusion: 2-year follow-upwardly report. J Neurosurg Spine 4(half-dozen):447–453. https://doi.org/10.3171/spi.2006.4.6.447
-
Furlan Advertizement, Pennick V, Bombardier C, van Tulder M (2009) 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 34(xviii):1929–1941. https://doi.org/ten.1097/BRS.0b013e3181b1c99f
-
Ostelo RW, Deyo RA, Stratford P, Waddell M, Croft P, Von Korff 1000, Bouter LM, de Vet HC (2008) Interpreting alter scores for pain and functional status in depression back pain: towards international consensus regarding minimal important change. Spine 33(1):90–94. https://doi.org/10.1097/BRS.0b013e31815e3a10
-
Orief T, Ramadan I, Seddik Z, Kamal K, Rahmany M, Takayasu 1000 (2010) Comparative evaluation of bone-filled Polymethylmethacrylate implant, autograft fusion, and Polyetheretherketone cervical cage fusion for the treatment of unmarried -level cervical disc disease. Asian J Neurosurg 5(2):46–56
-
Acharya S, Kumar S, Srivastava A, Tandon R (2011) Early on results of ane-level cervical discectomy and fusion with stand-alone cervical cage and os marrow soaked tricalcium phosphate. Acta Orthop Belg 77(2):218–223
-
Baskin DS, Ryan P, Sonntag V, Westmark R, Widmayer MA (2003) A prospective, randomized, controlled cervical fusion report using recombinant homo os morphogenetic protein-2 with the CORNERSTONE-SR allograft ring and the ATLANTIS inductive cervical plate. Spine 28(12):1219–1224. https://doi.org/ten.1097/01.brs.0000065486.22141.ca (discussion 1225)
-
Bhadra AK, Raman Equally, Casey AT, Crawford RJ (2009) Single-level cervical radiculopathy: clinical effect and cost-effectiveness of four techniques of anterior cervical discectomy and fusion and disc arthroplasty. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 18(two):232–237. https://doi.org/10.1007/s00586-008-0866-8
-
Chang-Jung C, Yi-Jie K, Yueh-Feng C, Rau M, Yang-Hwei T (2008) Inductive cervical fusion using a polyetheretherketone cage containing a bovine xenograftp: three to five-year follow-up. Spine 33(23):2524–2528
-
Chen JF, Wu CT, Lee SC, Lee ST (2005) Use of a polymethylmethacrylate cervical cage in the treatment of single-level cervical disc illness. J Neurosurg Spine 3(ane):24–28. https://doi.org/10.3171/spi.2005.3.one.0024
-
Chen JF, Wu CT, Lee ST (2009) The use of a hollow polymethylmethacrylate cervical spacer with plating in the handling of single level cervical disc disease. Chang Gung Med J 32(4):447–454
-
Cho DY, Lee WY, Sheu PC, Chen CC (2005) Cage containing a biphasic calcium phosphate ceramic (Triosite) for the treatment of cervical spondylosis. Surg Neurol 63(6):497–503. https://doi.org/10.1016/j.surneu.2004.ten.016 (discussion 494–503)
-
Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, Chiou TL, Chang YL, Su CF, Lin SZ, Chen SY (2008) Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci Off J Neurosurg Soc Australas 15(xi):1240–1245. https://doi.org/10.1016/j.jocn.2007.05.016
-
Dai LY, Jiang LS (2008) Anterior cervical fusion with interbody cage containing beta-tricalcium phosphate augmented with plate fixation: a prospective randomized study with 2-year follow-up. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 17(v):698–705. https://doi.org/x.1007/s00586-008-0643-8
-
Debusscher F, Aunoble S, Alsawad Y, Cloudless D, Le Huec JC (2009) Anterior cervical fusion with a bio-resorbable blended cage (beta TCP-PLLA): clinical and radiological results from a prospective study on 20 patients. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc xviii(9):1314–1320. https://doi.org/10.1007/s00586-009-1062-1
-
Fiere V, Greff G, Mosnier T, Faline A (2013) New cervical compressive staple: in vitro testing and early clinical results. J Spinal Disord Techn 26(7):385–392. https://doi.org/10.1097/BSD.0b013e31824a03d2
-
Grasso G, Giambartino F, Tomasello Thou, Iacopino Thou (2014) Inductive cervical discectomy and fusion with ROI-C peek cage: cervical alignment and patient outcomes. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 23(Suppl 6):650–657. https://doi.org/10.1007/s00586-014-3553-y
-
Gu Y, Yang HL, Chen L, Dong RB, Han GS, Wu GZ, Chen KW, Tang TS (2009) Use of an integrated anterior cervical plate and muzzle device (PCB) in cervical inductive fusion. J Clin Neurosci Off J Neurosurg Soc Australas 16(xi):1443–1448. https://doi.org/10.1016/j.jocn.2009.02.025
-
Ha BY, Sim HB, Lyo IU, Park ES, Kwon SC, Park JB (2012) Comparisons of two-level discectomy and fusion with cage lonely versus unmarried-level corpectomy and fusion with plate in the treatment of cervical degenerative disc disease. Korean J Spine 9(3):197–204. https://doi.org/10.14245/kjs.2012.ix.3.197
-
Iwasaki K, Ikedo T, Hashikata H, Toda H (2014) Autologous clavicle bone graft for inductive cervical discectomy and fusion with titanium interbody cage. J Neurosurg Spine 21(five):761–768. https://doi.org/ten.3171/2014.7.spine131000
-
Ji GY, Oh CH, Shin DA, Ha Y, Kim KN, Yoon DH, Yudoyono F (2015) Stand-alone cervical cages versus inductive cervical plates in 2-level cervical inductive interbody fusion patients. J Spinal Disord Techn 28(7):E433–E438
-
Kim Due south, Chun HJ, Yi HJ, Bak KH, Kim DW, Lee YK (2012) Long-term follow-up radiologic and clinical evaluation of cylindrical cage for anterior interbody fusion in degenerative cervical disc disease. J Korean Neurosurg Soc 52(ii):107–113
-
Kim SC, Kang SW, Kim SH, Cho KH, Kim SH (2009) Clinical and radiological outcomes of anterior cervical interbody fusion using hydroxyapatite spacer. J Korean Neurosurg Soc 46(4):300–304. https://doi.org/10.3340/jkns.2009.46.4.300
-
Lane PD, Cox JL, Gaskins RB 3rd, Santoni BG, Billys JB, Castellvi AE (2015) Early radiographic and clinical outcomes study evaluating an integrated spiral and interbody spacer for one- and 2-level ACDF. Int J Spine Surg 9:39. https://doi.org/x.14444/2039
-
Li J, Zheng Q, Guo 10, Zeng X, Zou Z, Liu Y, Hao Southward (2013) Anterior surgical options for the handling of cervical spondylotic myelopathy in a long-term follow-upwardly study. Curvation Orthop Trauma Surg 133(half dozen):745–751
-
Liao JC, Niu CC, Chen WJ, Chen LH (2008) Polyetheretherketone (PEEK) cage filled with cancellous allograft in inductive cervical discectomy and fusion. Int Orthop 32(5):643–648. https://doi.org/10.1007/s00264-007-0378-10
-
Liu J, Xiong X, Long X, Shu Y, Huang South, Yang D, Liu Z (2015) A new source of structural autograft for ACDF surgery: cervical laminae. Int J Clin Exp Med 8(6):9100–9106
-
Luo J, Huang S, Gong 1000, Li 50, Yu T, Zou 10 (2015) Two-level inductive cervical discectomy and fusion using self-locking stand-alone polyetheretherketone cages with two anchoring clips placed in the upper and lower vertebrae, respectively. Eur J Orthop Surg Traumatol Orthop Traumatol 25(Suppl ane):S147–S153. https://doi.org/10.1007/s00590-015-1613-vi
-
Mastronardi L, Ducati A, Ferrante 50 (2006) Anterior cervical fusion with polyetheretherketone (PEEK) cages in the treatment of degenerative disc illness. Preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir 148(3):307–312
-
Nagata T, Takami T, Yamagata T, Uda T, Naito K, Ohata K (2011) Significant relationship between local angle at fused segments and C2-7 angle: average duration of longer than 20 years later on inductive cervical discectomy and fusion. J Craniovertebral Junct Spine 2(two):62–66
-
Nemoto O, Kitada A, Naitou S, Tachibana A, Ito Y, Fujikawa A (2015) Stand-lone anchored cage versus cage with plating for single-level inductive cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol Orthop Traumatol 25(Suppl 1):S127–S134. https://doi.org/10.1007/s00590-014-1547-4
-
Niu CC, Liao JC, Chen WJ, Chen LH (2010) Outcomes of interbody fusion cages used in i and 2-levels inductive cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Techn 23(5):310–316. https://doi.org/10.1097/BSD.0b013e3181af3a84
-
Peelle MW, Rawlins BA, Frelinghuysen P (2007) A novel source of cancellous autograft for ACDF surgery: the manubrium. J Spinal Disord Techn twenty(1):36–41. https://doi.org/10.1097/01.bsd.0000211230.89554.5c
-
Ragab AA, Hodges FS, Colina CP, McGuire RA, Tucci M (2010) Dynamic anterior cervical plating for multi-level spondylosis: does information technology assist? Evid Based Spine-Care J 1(1):41–46. https://doi.org/ten.1055/south-0028-1100892
-
Ryu SI, Mitchell M, Kim DH (2006) A prospective randomized study comparison a cervical carbon fiber muzzle to the Smith-Robinson technique with allograft and plating: up to 24 months follow-up. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 15(ii):157–164. https://doi.org/10.1007/s00586-005-0951-1
-
Salame K, Ouaknine GE, Razon North, Rochkind S (2002) The use of carbon fiber cages in anterior cervical interbody fusion: report of 100 cases. Neurosurg Focus 12(1):E1. https://doi.org/ten.3171/foc.2002.12.ane.2
-
Samartzis D, Shen FH, Lyon C, Phillips K, Goldberg EJ, An HS (2004) Does rigid instrumentation increase the fusion charge per unit in one-level anterior cervical discectomy and fusion? Spine J Off J North Am Spine Soc four(half-dozen):636–643. https://doi.org/x.1016/j.spinee.2004.04.010
-
Sangala JR, Nichols T, Uribe JS, Melton Thousand, Vale FL (2010) Sternal cancellous os graft harvest for anterior cervical discectomy and fusion with interbody muzzle devices. Clin Neurol Neurosurg 112(6):470–473. https://doi.org/10.1016/j.clineuro.2010.03.011
-
Schils F, Rilliet B, Payer M (2006) Implantation of an empty carbon cobweb muzzle or a tricortical iliac crest autograft after cervical discectomy for unmarried-level disc herniation: a prospective comparative study. J Neurosurg Spine four(iv):292–299. https://doi.org/10.3171/spi.2006.4.4.292
-
Scholz Yard, Schnake KJ, Pingel A, Hoffmann R, Kandziora F (2011) A new zero-profile implant for stand-solitary inductive cervical interbody fusion. Clin Orthop Relat Res 469(3):666–673. https://doi.org/10.1007/s11999-010-1597-9
-
Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS (2004) Comparison of clinical and radiographic event in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J iv(6):629–635
-
Shin SH, Lee WJ, Eun JP, Choi HY, Lee JC (2007) Clinical and radiologic assessment for inductive cervical interbody fusion with synthetic cages. J Korean Neurosurg Soc 41(2):105–110
-
Siam AE, El Saghir H, El-Fiky T, Moustafa O, El Mansy Y (2014) Results of ACDF using Alexandria modular muzzle-plate construct in cervical canal stenosis. Eur Orthop Traumatol 5(two):131–137
-
Singh D, Sinha Due south, Singh H, Jagetia A, Gupta South, Gangoo P, Tandon 1000 (2011) Use of nitinol shape memory blend staples (NiTi clips) afterward cervical discoidectomy: minimally invasive instrumentation and long-term results. Minim Invasive Neurosurg MIN 54(4):172–178. https://doi.org/10.1055/south-0031-1284399
-
Song KJ, Lee KB (2006) A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci Off J Neurosurg Soc Australas 13(ii):181–187. https://doi.org/10.1016/j.jocn.2005.02.018
-
Sugawara T, Itoh Y, Hirano Y, Higashiyama North, Mizoi K (2011) beta-Tricalcium phosphate promotes bony fusion afterward anterior cervical discectomy and fusion using titanium cages. Spine 36(23):E1509–E1514. https://doi.org/10.1097/BRS.0b013e31820e60d9
-
Tan J, Zheng Y, Gong 50, Liu X, Li J, Du W (2008) Anterior cervical discectomy and interbody fusion by endoscopic approach: a preliminary report. J Neurosurg Spine 8(i):17–21. https://doi.org/x.3171/spi-08/01/017
-
Tancredi A, Agrillo A, Delfini R, Fiume D, Frati A, Rinaldi A (2004) Utilise of carbon fiber cages for treatment of cervical myeloradiculopathies. Surg Neurol 61(3):221–226. https://doi.org/10.1016/j.surneu.2003.07.014 (discussion 226)
-
Wang C, Zhang Y, Yuan W (2014) Early on clinical outcomes and radiographic features after handling of cervical degenerative disc illness with the new zero-profile implant: a one-year follow-up retrospective written report. J Spinal Disord Techn. https://doi.org/x.1097/bsd.0000000000000101
-
Wang MY, Liu CY (2005) Resorbable polylactic acrid interbody spacers with vertebral autograft for anterior cervical discectomy and fusion. Neurosurgery 57(1):135–140 (discussion 135–140)
-
Wang Ten, Chen Y, Chen D, Yuan W, Chen Ten, Zhou X, Xiao J, Ni B, Jia Fifty (2009) Inductive decompression and interbody fusion with BAK/C for cervical disc degenerative disorders. J Spinal Disord Techn 22(4):240–245. https://doi.org/ten.1097/BSD.0b013e31816d5f7e
-
Wang Z, Jiang W, Li X, Wang H, Shi J, Chen J, Meng B, Yang H (2014) The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J 24(1):148–154
-
Wang Z, Zhu R, Yang H, Shen K, Wang K, Chen K, Gan M, Li Chiliad (2015) Zero-profile implant (Zero-p) versus plate cage benezech implant (PCB) in the treatment of unmarried-level cervical spondylotic myelopathy. BMC Musculoskelet Disord 16:290. https://doi.org/ten.1186/s12891-015-0746-iv
-
Wei F, Wang 50, Zhou Z, Zhong R, Liu S, Cui S, Pan X, Gao Thou (2015) Cervical cage without plating in direction of type II/Ii A Hangman'due south fracture combined with intervertebral disc injury. BMC Musculoskelet Disord 16:285. https://doi.org/10.1186/s12891-015-0734-eight
-
Wilkinson JS, Mann SA, Stoneham GW, Hentschel S, Fourney DR (2011) Comparing of mail service-operative lordosis with the PEEK cage and the cervical plate. Can J Neurol Sci Le J Tin can des Sci Neurol 38(1):72–77
-
Woiciechowsky C, Thomale UW, Kroppenstedt SN (2004) Degenerative spondylolisthesis of the cervical spine—symptoms and surgical strategies depending on illness progress. Eur Spine J 13(8):680–684
-
Wu WJ, Jiang LS, Liang Y, Dai LY (2012) Muzzle subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 21(7):1374–1382. https://doi.org/10.1007/s00586-011-2131-9
-
Xie Y, Li H, Yuan J, Fu L, Yang J, Zhang P (2015) A prospective randomized comparison of PEEK cage containing calcium sulphate or demineralized os matrix with autograft in anterior cervical interbody fusion. Int Orthop 39(six):1129–1136. https://doi.org/10.1007/s00264-014-2610-9
-
Yan D, Li J, Zhang Z (2014) Anterior cervical discectomy and fusion with the zero-profile implant system for cervical spondylotic myelopathy. Techn Orthop 29(1):49–53
-
Yan JL, Chen JF, Lee ST, Chang CN, Liao CC (2014) Surgical outcomes of Cervios ChronOS cage implantation for degenerative cervical Intervertebral deejay disorder. Neurosurg Q 24(3):161–166
-
Yang L, Gu Y, Liang L, Gao R, Shi S, Shi J, Yuan Due west (2012) Stand-lonely anchored spacer versus anterior plate for multilevel anterior cervical diskectomy and fusion. Orthopedics 35(10):e1503–e1510. https://doi.org/x.3928/01477447-20120919-twenty
-
Yao N, Wang C, Wang W, Wang L (2011) Full-endoscopic technique for inductive cervical discectomy and interbody fusion: 5-year follow-upward results of 67 cases. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 20(vi):899–904. https://doi.org/10.1007/s00586-010-1642-0
-
Zagra A, Zagra L, Scaramuzzo Fifty, Minoia L, Archetti M, Giudici F (2013) Anterior cervical fusion for radicular-disc conflict performed by three different procedures: clinical and radiographic analysis at long-term follow-up. Eur Spine J 22:S905–S909
-
Zhou J, Xia Q, Dong J, Li X, Zhou X, Fang T, Lin H (2011) Comparison of stand-alone polyetheretherketone cages and iliac crest autografts for the treatment of cervical degenerative disc diseases. Acta Neurochir 153(1):115–122. https://doi.org/ten.1007/s00701-010-0821-4
-
Chang MY, Chen MH, Chang CJ, Huang JS (2013) Preliminary clinical experience with polyetheretherketone cages filled with synthetic crystallic semihydrate form of calcium sulfate for inductive cervical discectomy and fusion. Formos J Surg 46(four):109–115
-
Cho HJ, Hur JW, Lee JB, Han JS, Cho Th, Park JY (2015) Cervical stand up-lonely polyetheretherketone cage versus naught-profile anchored spacer in single-level inductive cervical discectomy and fusion: minimum 2-year assessment of radiographic and clinical effect. J Korean Neurosurg Soc 58(2):119–124. https://doi.org/10.3340/jkns.2015.58.2.119
-
Eastlack RK, Garfin SR, Brown CR, Meyer SC (2014) Osteocel Plus cellular allograft in anterior cervical discectomy and fusion: evaluation of clinical and radiographic outcomes from a prospective multicenter study. Spine 39(22):E1331–E1337. https://doi.org/ten.1097/brs.0000000000000557
-
El-Tantawy A (2015) Is it possible to eliminate the plate-related problems and still achieve satisfactory outcome later on multilevel anterior cervical discectomy? Eur J Orthop Surg Traumatol Orthop Traumatol 25(Suppl 1):S135–S145. https://doi.org/10.1007/s00590-015-1611-8
-
Farrokhi MR, Nikoo Z, Gholami M, Hosseini K (2015) Comparison between acrylic muzzle and polyetheretherketone (PEEK) muzzle in single-level inductive cervical discectomy and fusion: a randomized clinical trial. J Spinal Disord Techn. https://doi.org/10.1097/bsd.0000000000000251
-
Fernandez-Fairen M, Sala P, Dufoo G Jr, Ballester J, Murcia A, Merzthal Fifty (2008) Anterior cervical fusion with tantalum implant: a prospective randomized controlled study. Spine 33(5):465–472
-
Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL (2000) A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine 25(20):2646–2654 (discussion 2655)
-
Hofstetter CP, Kesavabhotla Thou, Boockvar JA (2015) Zero-profile anchored spacer reduces charge per unit of dysphagia compared with ACDF with anterior plating. J Spinal Disord Techn 28(5):E284–E290. https://doi.org/10.1097/BSD.0b013e31828873ed
-
Kim CH, Chung CK, Hahn S (2013) Autologous iliac bone graft with anterior plating is advantageous over the stand up-solitary cage for segmental lordosis in single-level cervical disc disease. Neurosurgery 72(ii):257–265. https://doi.org/ten.1227/neu.0b013e31827b94d4 (discussion 266)
-
Lee CH, Kim KJ, Hyun SJ, Yeom JS, Jahng TA, Kim HJ (2015) Subsidence as of 12 months after single-level anterior cervical inter-body fusion. Is it related to clinical outcomes? Acta Neurochir 157(6):1063–1068. https://doi.org/10.1007/s00701-015-2388-vi
-
Mashhadinezhad H, Samini F, Zare R (2014) Comparison of outcomes and safety of using hydroxyapatite granules equally a substitute for autograft in cervical cages for anterior cervical discectomy and interbody fusion. Arch Bone Joint Surg 2(1):37–42
-
Mobbs RJ, Rao P, Chandran NK (2007) Anterior cervical discectomy and fusion: analysis of surgical upshot with and without plating. J Clin Neurosci Off J Neurosurg Soc Australas 14(7):639–642. https://doi.org/10.1016/j.jocn.2006.04.003
-
Oh HS, Shim CS, Kim JS, Lee SH (2013) Clinical and radiological comparison of femur and fibular allografts for the treatment of cervical degenerative disc diseases. J Korean Neurosurg Soc 53(one):vi–12. https://doi.org/x.3340/jkns.2013.53.1.6
-
Park JH, Roh SW (2013) Anterior cervical interbody fusion using polyetheretherketone cage filled with autologous and synthetic os graft substrates for cervical spondylosis: comparative analysis betwixt polybone and iliac bone. Neurol Med Chir 53(ii):85–xc
-
Pourtaheri S, Hwang K, Faloon M, Issa Thou, Mease SJ, Mangels D, Sinha Thou, Emami A (2015) Ultra-depression-dose recombinant man bone morphogenetic poly peptide-two for iii-level anterior cervical diskectomy and fusion. Orthopedics 38(4):241–245
-
Saphier PS, Arginteanu MS, Moore FM, Steinberger AA, Camins MB (2007) Stress-shielding compared with load-sharing anterior cervical plate fixation: a clinical and radiographic prospective analysis of fifty patients. J Neurosurg Spine 6(v):391–397. https://doi.org/10.3171/spi.2007.6.5.391
-
Scholz Chiliad, Schelfaut S, Pingel A, Schleicher P, Kandziora F (2014) A cervical "aught-profile" cage with integrated angle-stable fixation: 24-months results. Acta Orthop Belg eighty(4):558–566
-
Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA (2005) Use of the Solis cage and local autologous os graft for anterior cervical discectomy and fusion: early technical experience. J Neurosurg Spine 2(2):116–122. https://doi.org/x.3171/spi.2005.2.2.0116
-
Vocal J, Taghavi CE, Hsu DW, Vocal KJ, Song JH, Lee KB (2012) Radiological changes in anterior cervical discectomy and fusion with muzzle and plate construct: the significance of the anterior spur formation sign. Spine 37(4):272–279. https://doi.org/10.1097/BRS.0b013e31821c3cbf
-
Song KJ, Taghavi CE, Hsu MS, Lee KB, Kim GH, Song JH (2010) Plate augmentation in anterior cervical discectomy and fusion with muzzle for degenerative cervical spinal disorders. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 19(10):1677–1683. https://doi.org/10.1007/s00586-010-1283-3
-
Vocal KJ, Taghavi CE, Lee KB, Song JH, Eun JP (2009) The efficacy of plate construct augmentation versus cage alone in inductive cervical fusion. Spine 34(26):2886–2892. https://doi.org/10.1097/BRS.0b013e3181b64f2c
-
Suchomel P, Barsa P, Buchvald P, Svobodnik A, Vanickova East (2004) Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion: a prospective study with respect to bone union pattern. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc thirteen(half-dozen):510–515. https://doi.org/10.1007/s00586-003-0667-z
-
Tabaraee E, Ahn J, Bohl DD, Elboghdady IM, Aboushaala M, Singh K (2015) The bear upon of worker's compensation claims on outcomes and costs following an anterior cervical discectomy and fusion. Spine 40(12):948–953. https://doi.org/ten.1097/brs.0000000000000873
-
Takeuchi 1000, Yasuda Thou, Niwa A, Wakao N, Nakura T, Osuka K, Kamiya M, Takayasu One thousand (2014) Plasmapore-coated titanium cervical cages induce more rapid and complete bone fusion after anterior cervical discectomy and fusion every bit compared to noncoated titanium cages. Earth Neurosurg 82(three–4):519–522. https://doi.org/10.1016/j.wneu.2013.04.001
-
Tomasino A, Gebhard H, Parikh Thou, Wess C, Hartl R (2009) Bioabsorbable instrumentation for single-level cervical degenerative disc disease: a radiological and clinical outcome report. J Neurosurg Spine 11(v):529–537. https://doi.org/10.3171/2009.6.spine08838
-
Topuz Thou, Colak A, Kaya South, Simsek H, Kutlay M, Demircan MN, Velioglu M (2009) Two-level face-to-face cervical disc affliction treated with peek cages packed with demineralized bone matrix: results of three-twelvemonth follow-up. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 18(two):238–243. https://doi.org/ten.1007/s00586-008-0869-v
-
Vanek P, Bradac O, DeLacy P, Lacman J, Benes V (2013) Anterior interbody fusion of the cervical spine with zero-P spacer: prospective comparative report—clinical and radiological results at a minimum 2 years later surgery. Spine 38(xiii):E792–E797
-
Wang 60 minutes, Li XL, Dong J, Yuan FL, Zhou J (2013) Skip-level anterior cervical discectomy and fusion with self-locking stand-alone PEEK cages for the treatment of 2 noncontiguous levels of cervical spondylosis. J Spinal Disord Techn 26(7):E286–E292. https://doi.org/x.1097/BSD.0b013e31828679b3
-
Yi J, Lee GW, Nam WD, Han KY, Kim MH, Kang JW, Won J, Kim SW, Noh W, Yeom JS (2015) A prospective randomized clinical trial comparing bone matrimony rate following anterior cervical discectomy and fusion using a polyetheretherketone cage: hydroxyapatite/b-tricalcium phosphate mixture versus hydroxyapatite/demineralized os matrix mixture. Asian Spine J 9(ane):thirty–38. https://doi.org/ten.4184/asj.2015.nine.one.thirty
-
Zigler JE, Delamarter R, Murrey D, Spivak J, Janssen M (2013) ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease: five-yr results of a Food and Drug Assistants report. Spine 38(3):203–209. https://doi.org/10.1097/BRS.0b013e318278eb38
-
Coric D, Kim PK, Clemente JD, Boltes MO, Nussbaum M, James S (2013) Prospective randomized report of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. J Neurosurg Spine 18(ane):36–42. https://doi.org/10.3171/2012.nine.spine12555
-
Hauerberg J, Kosteljanetz M, Boge-Rasmussen T, Dons K, Gideon P, Springborg JB, Wagner A (2008) Anterior cervical discectomy with or without fusion with ray titanium muzzle: a prospective randomized clinical study. Spine 33(five):458–464. https://doi.org/10.1097/BRS.0b013e3181657dac
-
Hellbusch LC, Spangler WJ, Bowder A (2012) Radiographic PEEK double-lucency finding afterwards anterior cervical discectomy and fusion with local autograft and PEEK spacer: a preliminary report. J Neurosurg Spine 16(3):248–250. https://doi.org/10.3171/2011.eleven.spine1141
-
Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, Coric D, Cauthen JC, Riew DK (2009) Comparison of BRYAN cervical disc arthroplasty with inductive cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine 34(2):101–107. https://doi.org/10.1097/BRS.0b013e31818ee263
-
Jagannathan J, Shaffrey CI, Oskouian RJ, Dumont AS, Herrold C, Sansur CA, Jane JA (2008) Radiographic and clinical outcomes post-obit single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. J Neurosurg Spine 8(5):420–428. https://doi.org/10.3171/spi/2008/eight/5/420
-
Joo YH, Lee JW, Kwon KY, Rhee JJ, Lee HK (2010) Comparing of fusion with muzzle lonely and plate instrumentation in ii-level cervical degenerative disease. J Korean Neurosurg Soc 48(4):342–346. https://doi.org/ten.3340/jkns.2010.48.4.342
-
Marbacher S, Hidalgo-Staub T, Kienzler J, Wuergler-Hauri C, Landolt H, Fandino J (2015) Long-term outcome after adjacent ii-level anterior cervical discectomy and fusion using stand-alone plasmaphore-covered titanium cages. J Neurol Surg Part A Central Eur Neurosurg 76(3):199–204. https://doi.org/10.1055/s-0034-1382782
-
Moon HJ, Kim JH, Kim JH, Kwon Th, Chung HS, Park YK (2011) The effects of inductive cervical discectomy and fusion with stand-lone cages at 2 contiguous levels on cervical alignment and outcomes. Acta Neurochir 153(three):559–565. https://doi.org/10.1007/s00701-010-0879-z
-
Oh JK, Kim TY, Lee HS, You NK, Choi GH, Yi S, Ha Y, Kim KN, Yoon DH, Shin HC (2013) Stand-alone cervical cages versus anterior cervical plate in 2-level cervical anterior interbody fusion patients: clinical outcomes and radiologic changes. J Spinal Disord Techn 26(viii):415–420. https://doi.org/10.1097/BSD.0b013e31824c7d22
-
Ramzi N, Ribeiro-Vaz G, Fomekong E, Lecouvet Atomic number 26, Raftopoulos C (2008) Long term outcome of anterior cervical discectomy and fusion using coral grafts. Acta Neurochir 150(12):1249–1256. https://doi.org/10.1007/s00701-008-0140-1 (discussion 1256)
-
Tureyen K, Maciejczak A (2003) Disc height loss subsequently anterior cervical microdiscectomy with titanium intervertebral cage fusion. Acta Neurochir 145(7):565–570
-
Klingler JH, Kruger MT, Sircar R, Kogias Eastward, Scholz C, Volz F, Scheiwe C, Hubbe U (2014) PEEK cages versus PMMA spacers in anterior cervical discectomy: comparison of fusion, subsidence, sagittal alignment, and clinical event with a minimum one-year follow-up. Sci World J 2014:398396. https://doi.org/x.1155/2014/398396
-
Pechlivanis I, Thuring T, Brenke C, Seiz M, Thome C, Barth M, Harders A, Schmieder K (2011) Non-fusion rates in anterior cervical discectomy and implantation of empty polyetheretherketone cages. Spine 36(1):xv–xx. https://doi.org/x.1097/BRS.0b013e3181cbf870
-
Yoshii T, Yuasa M, Sotome Due south, Yamada T, Sakaki 1000, Hirai T, Taniyama T, Inose H, Kato T, Arai Y, Kawabata S, Tomizawa S, Enomoto M, Shinomiya Thousand, Okawa A (2013) Porous/dense composite hydroxyapatite for anterior cervical discectomy and fusion. Spine 38(10):833–840. https://doi.org/10.1097/BRS.0b013e3182801390
-
Cabraja M, Oezdemir S, Koeppen D, Kroppenstedt S (2012) Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord xiii:172. https://doi.org/10.1186/1471-2474-xiii-172
-
Njoku I, Alimi M, Leng LZ, Shin BJ, James AR, Bhangoo S, Tsiouris AJ, Hartl R (2014) Inductive cervical discectomy and fusion with a nil-profile integrated plate and spacer device: a clinical and radiological study. J Neurosurg Spine 21(4):529–537
-
Tani S, Nagashima H, Isoshima A, Akiyama Thou, Ohashi H, Tochigi S, Abe T (2010) A unique device, the disc infinite-fitted lark device, for anterior cervical discectomy and fusion: early clinical and radiological evaluation. J Neurosurg Spine 12(iv):342–346. https://doi.org/10.3171/2009.10.spine09283
-
Thome C, Leheta O, Krauss JK, Zevgaridis D (2006) A prospective randomized comparing of rectangular titanium cage fusion and iliac crest autograft fusion in patients undergoing anterior cervical discectomy. J Neurosurg Spine 4(one):1–nine. https://doi.org/10.3171/spi.2006.4.1.1
-
Yoo M, Kim WH, Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2014) Comparing between two unlike cervical interbody fusion cages in one level stand-alone ACDF: carbon fiber composite frame muzzle versus polyetheretherketone cage. Korean J Spine 11(3):127–135. https://doi.org/10.14245/kjs.2014.xi.three.127
-
Choi MK, Kim SB, Park CK, Kim SM (2016) Comparison of the clinical and radiologic outcomes obtained with single- versus ii-level anterior cervical decompression and fusion using stand up-alone PEEK cages filled with allograft. Acta Neurochir. https://doi.org/x.1007/s00701-015-2692-1
-
Nunley PD, Jawahar A, Kerr EJ tertiary, Cavanaugh DA, Howard C, Brandao SM (2009) Selection of plate may touch outcomes for single versus multilevel ACDF: results of a prospective randomized single-blind trial. Spine J Off J North Am Spine Soc 9(2):121–127. https://doi.org/x.1016/j.spinee.2007.11.009
-
Park JI, Cho DC, Kim KT, Sung JK (2013) Anterior cervical discectomy and fusion using a stand-alone polyetheretherketone cage packed with local autobone: cess of bone fusion and subsidence. J Korean Neurosurg Soc 54(3):189–193. https://doi.org/10.3340/jkns.2013.54.three.189
-
Schroder J, Grosse-Dresselhaus F, Schul C, Wassmann H (2007) Anterior cervical spinal fusion with the Intromed ZWE System: preliminary experience. Neurosurg Rev thirty(1):63–68. https://doi.org/x.1007/s10143-006-0043-vii (discussion 68)
-
Shiban E, Gapon K, Wostrack Grand, Meyer B, Lehmberg J (2015) Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir. https://doi.org/ten.1007/s00701-015-2630-2
-
Wright IP, Eisenstein SM (2007) Anterior cervical discectomy and fusion without instrumentation. Spine 32(7):772–774. https://doi.org/10.1097/01.brs.0000258846.86537.ad (word 775)
-
Zhou J, Li X, Dong J, Zhou X, Fang T, Lin H, Ma Y (2011) Iii-level anterior cervical discectomy and fusion with self-locking stand-lone polyetheretherketone cages. J Clin Neurosci Off J Neurosurg Soc Australas 18(11):1505–1509. https://doi.org/x.1016/j.jocn.2011.02.045
-
Ouchida J, Yukawa Y, Ito K, Machino One thousand, Inoue T, Tomita Thou, Kato F (2015) Functional computed tomography scanning for evaluating fusion condition after anterior cervical decompression fusion. v 24(12):2924–2929. https://doi.org/x.1007/s00586-014-3722-z
-
Johnsson R, Stromqvist B, Aspenberg P (2002) Randomized radiostereometric study comparison osteogenic protein-one (BMP-7) and autograft bone in human noninstrumented posterolateral lumbar fusion: 2002 Volvo Award in clinical studies. Spine 27(23):2654–2661. https://doi.org/ten.1097/01.brs.0000035339.83704.60
Author information
Affiliations
Corresponding writer
Ethics declarations
Disharmonize of interest
All authors declare that they take no conflict of interest.
Electronic supplementary material
Rights and permissions
Open Admission This commodity is distributed nether the terms of the Artistic Eatables Attribution four.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(due south) and the source, provide a link to the Creative Commons license, and betoken if changes were made.
Reprints and Permissions
Nigh this article
Cite this article
Noordhoek, I., Koning, M.T. & Vleggeert-Lankamp, C.50.A. Evaluation of bony fusion subsequently anterior cervical discectomy: a systematic literature review. Eur Spine J 28, 386–399 (2019). https://doi.org/10.1007/s00586-018-5820-9
-
Received:
-
Accepted:
-
Published:
-
Effect Engagement:
-
DOI : https://doi.org/10.1007/s00586-018-5820-9
Keywords
- Anterior cervical discectomy and fusion
- Radiologic techniques
- Speed of fusion
- Clinical outcome
Source: https://link.springer.com/article/10.1007/s00586-018-5820-9
0 Response to "How Do You Know if Your Acdf Implant Didnt Take"
Post a Comment